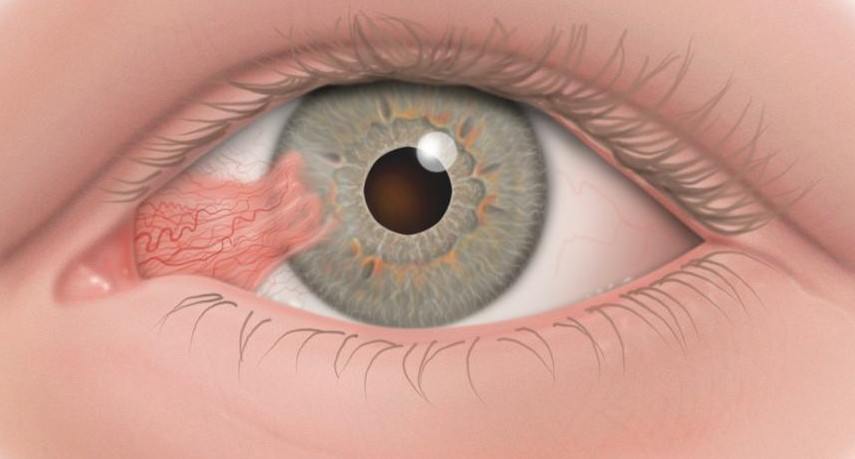
A pterygium is a triangular growth of abnormal conjunctival tissue that invades the cornea.
Its development is not related to injury or inflammation. 90% of pterygia are located nasally, the nose side of the eye. Both eyes are frequently involved but often only one.
The pterygium can advance to involve the visual axis causing marked loss of visual acuity.
The pterygium can be distinguished from a pingueculum, which is a small-elevated yellowish mass, which can become inflamed. The pterygium grows in the interpalpebral fissure (that is the exposed part of the eye) as an elevated fleshy mass of the conjunctiva.
Symptoms
Burning, irritation, tearing and a foreign body sensation may accompany the growth of a pterygium onto a cornea. Astigmatism may be induced and may lead to decreased vision. As the apex of the pterygium approaches the visual axis, glare and reduced contrast sensitivity appear.
For poorly understood reasons the pterygium growth may stop at any stage. It may remain so for the rest of the patient’s life or at a later date again start growing.
Etiology and Epidemiology
There is a worldwide distribution of pterygium but it is more common in warm, dry climates. Studies have shown a strong relationship between ultraviolet radiation and the formation of pterygia.
A study in Australia identified a number of risk factors:
- Living in the tropics
- Working in a sandy outdoor environment
- Not wearing sunglasses
- Not wearing a hat
Local drying of the conjunctiva and tearfilm abnormalities may also be contributing factors.
The highest incidents occur between the ages of 20-49 and rarely occur under the age of 15.
Treatment
The decision to remove a pterygium is dependent on the patient’s symptoms, complications caused by the pterygium and the interest in cosmetic improvement. Recurrences may be more frequent in young adults. Virtually all post-operative recurrences occur within the first year after surgery and often within 6-8 weeks. With recurrence there is a higher incidence of growth into the visual axis.
Medical Treatment
Eye drops such as preservative free lubricants, vasoconstrictors and mild corticosteroids can relive the symptoms. Some believe ultraviolet-blocking spectacles can prevent progression.
Surgical
The pterygium is removed surgically and the method depends on the surgeon doing the operation.
- The pterygium is avulsed.
- The pterygium is excised and the underlined sclera is left exposed, that is bare sclera.
- Transplantation of the head of the pterygium away from the cornea beneath the superior edge of the adjacent normal conjunctiva.
- Keratectomy, is when a superficial layer of the cornea is removed during the pterygium operation on the cornea. The pterygium may then be removed, and the sclera left bare as above or the head of the pterygium can be transplanted.
Adjunctive Therapy
A number of therapies are used to decrease the risk of recurrence after surgical removal of the pterygium. The treatment used again depends on the surgeon’s preference. Each has attractive features, but none is without drawbacks.
The following may be used:
- Steroid drops.
- Thiotepa, a radiomimetic agent, which presumably obliterates proliferation of vascular cells and is very rarely used today.
- Mitomycen C is an antineoplastic-antibiotic agent, which inhibits the synthesis of proteins.
- Beta-radiation. Strontium-90 applicators are used to radiate the site of the pterygium after surgical removal.
- Performing an auto-graft in which a piece of conjunctiva from the same eye is glued or sutured onto the site that the pterygium was removed.
Future Prospects
The first report of a surgical treatment of a pterygium is more than 3000 years old. The management of pterygia and recurrent pterygia is improving yet many questions remain unanswered. Future studies may elucidate the cause of the pterygium as well as the cause of complications related to the adjunctive therapy after pterygium surgery and prevent recurrence.