FOR THIS ARTICLE, NDSS INTERVIEWED DANIELLE LEDOUX, MD ASSISTANT IN OPHTHALMOLOGY AT CHILDREN’S HOSPITAL, BOSTON AND INSTRUCTOR IN OPHTHALMOLOGY AT HARVARD MEDICAL SCHOOL
Down syndrome has effects on the developing eye which can impact the proper development of vision. Eye disease is reported in over half of patients with Down Syndrome, from less severe problems such as tear duct abnormalities to vision threatening diagnoses such as the early onset of cataracts. Particular attention should be paid to vision in people with Down syndrome.
What is Different About the Eyes in Individuals with Down Syndrome?
Dr. Ledoux: As any family member of a person with Down syndrome knows, there are characteristic features about the eyes. This includes upward slanting of the eyelids, prominent folds of skin between the eye and the nose, and small white spots present on the iris (the coloured part of the eye) called Brushfield’s spots. These spots are harmless.
Do Most Children with Down Syndrome Need Glasses?
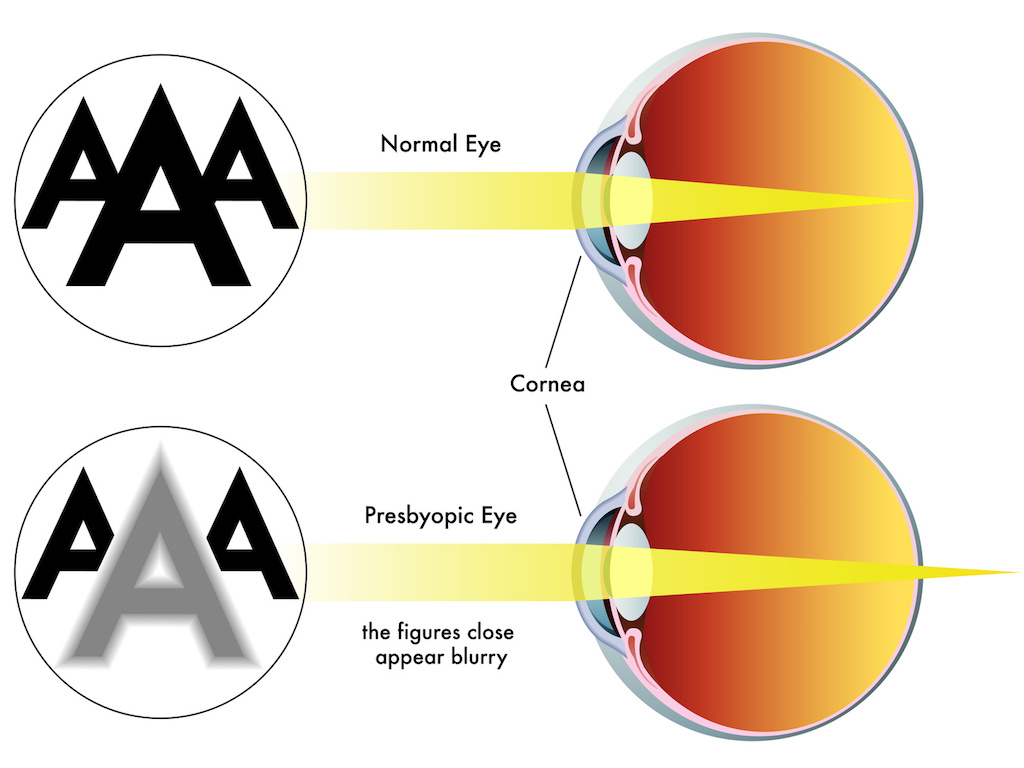
Dr. Ledoux: Refractive error (the need for glasses) is much more common in children with Down syndrome than in the general population. This refractive error can be hyperopia (farsightedness), astigmatism, or myopia (nearsightedness). Another problem is weak accommodation (difficulty changing the focusing power of the eye from distance to near). We can test this easily in the office, and if detected, we will prescribe glasses that have bifocals. Some of my patients have difficulty adjusting to glasses, but once they get accustomed to having the glasses on their face, their vision is significantly better and often their eye alignment improves as well.
What Are Common, but Less Serious, Eye Abnormalities Affecting Patients with Down Syndrome?
Dr. Ledoux: In addition to the need for eyeglasses, many children with Down syndrome have tear duct abnormalities. Family members will notice this as frequent discharge and tearing from the eyes, worsened by colds. We generally recommend firm massage over the space and down towards the nose (tear sac region) 2-3 times a day to attempt to open the tear duct. If this continues beyond 1-2 years of age, the tear ducts may need to be opened by a surgical procedure.
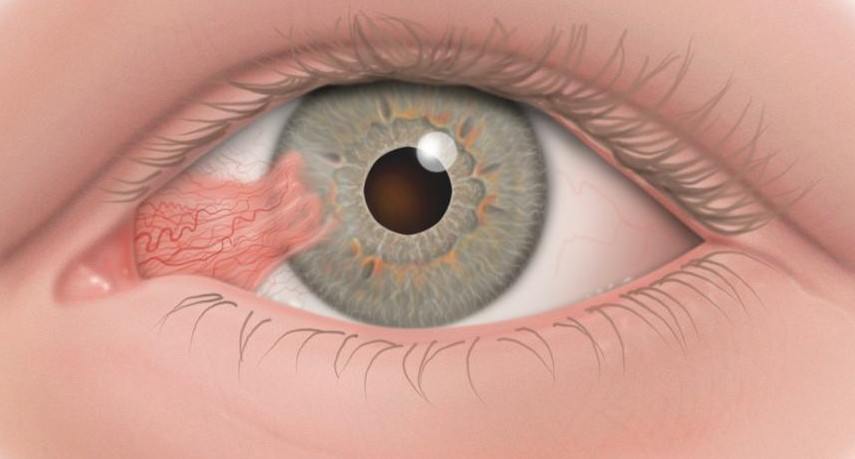
Strabismus (eye misalignment/ squint) is also more common. Family members may notice that the eyes do not line up well with each other, but often the strabismus can be subtle, even to the pediatrician. The folds of skin I mentioned between the eyes and the nose can also cover up the underlying strabismus, or make the eyes appear as if they are crossing even if they are not. It is important to diagnose strabismus as a child, as crossed eyes can result in amblyopia (loss of vision also known as lazy eye) and loss of stereopsis (the use of the two eyes together or depth perception).
How Can the Strabismus Be Treated?
Dr. Ledoux: Sometimes, simply glasses alone are enough to straighten eyes with strabismus. If glasses are needed, we always start there. If the eyes continue to have strabismus despite the correct pair of eyeglasses, then we recommend strabismus surgery (eye muscle surgery). This is a one to two hour procedure. Unfortunately, our patients with Down syndrome are more likely to require more than one surgery to align their eyes as they don’t always respond as predictably to strabismus surgery as the general population with strabismus would.
What Are the More Severe Eye Problems That Might Develop?
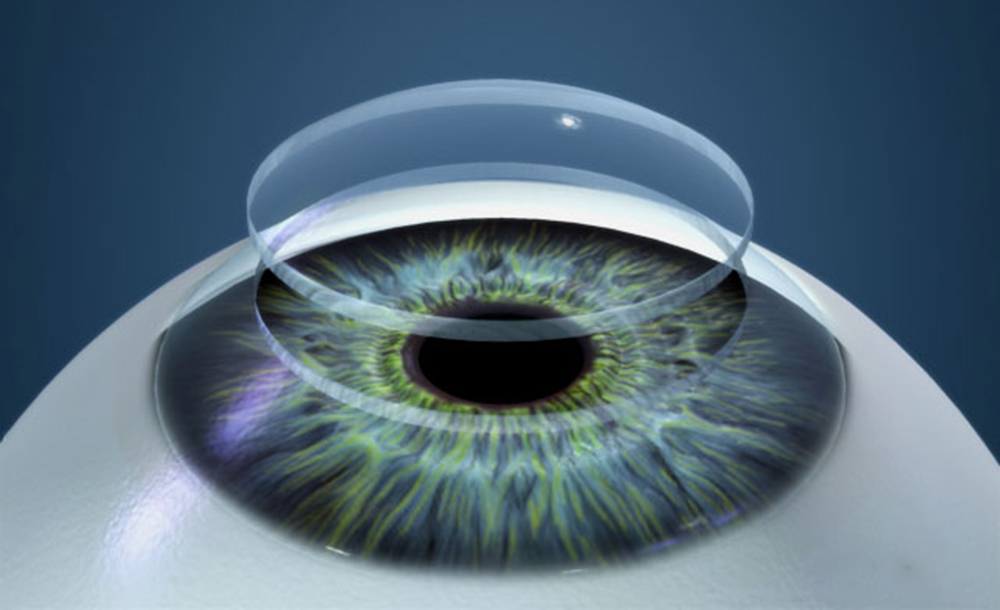
Dr. Ledoux: My greatest concern is congenital cataracts (lack of clearness to the lens of the eye). If visually significant cataracts are present early in a child’s eye, then a clear image is not delivered to the brain and therefore the brain can never “learn” to see. This is a severe form of amblyopia known as form deprivation amblyopia. While we can take our time removing a cataract in an adult patient, if significant cataracts are present very early in a child’s life, and not removed, can result in lifelong poor vision. In that situation, even if the cataract is removed when the child is older, the vision never improves significantly. This is what makes early detection of cataracts in infants and children so important. A child with Down syndrome will be evaluated by the paediatrician at birth, and referred to an ophthalmologist if something abnormal is detected. There is also a unique form of cataract in Down syndrome patients that we have found in our research. However, depending on how developmentally delayed the person is, they may not be able to communicate that they can’t see. For this reason, I recommend any patient with Down syndrome, no matter what age, have a complete eye examination if they are starting to show reduced cognitive function, or changes in their normal activities.
Are There Other Eye Conditions in Down Syndrome That Can Cause Loss of Eyesight?
Dr. Ledoux: I mentioned amblyopia (commonly called “lazy eye” which is decreased vision) which can be caused by multiple different eye problems such as strabismus, severe ptosis (eyelid droop), cataracts, or even uncorrected refractive error, especially if one eye needs a much stronger eyeglass prescription than the other. Ptosis is usually easier to appreciate but strabismus and significant refractive error can be very difficult for the paediatrician to diagnose. There are other more rare problems which can occur with the optic nerve or retina of the eye which can sometimes cause vision loss and unfortunately are generally not treatable. Nystagmus (a rhythmic shaking of the eyes) can also occur.
What is the Recommended Eye Care for Children with Down Syndrome?
Dr. Ledoux: The American Academy of Paediatrics (AAP) and the Down Syndrome Medical Interest Group (DSMIG) recommend evaluation of the red reflex of the eyes at birth to look for cataracts, as well as to assess the eyes for strabismus or nystagmus. The red reflex is essentially the “red eye” seen in photographs, which is the normal reflex of the retina when struck by direct light. If the eyes don’t look normal, then the infant will be referred to a paediatric ophthalmologist – a physician who has completed specialty training in medical and surgical management of the child’s eye. We, along with the AAP and the DSMIG, recommend a child with Down syndrome has their first eye exam by an ophthalmologist experienced in patients with special disabilities (for example, a paediatric ophthalmologist) by six months of age. After that, children with Down syndrome, even if they are without symptoms, should see an ophthalmologist every one to two years. If any eye problems are detected, they will be followed more frequently.
What Sort of Symptoms Might We See If a Child Has an Eye Problem?
Dr. Ledoux: Unfortunately, children with Down Syndrome often do not complain about their eye problems, either because they don’t notice the problem or because they can’t communicate the problem well enough. Signs to look for include squinting or closing one eye shut, an unusual head tilt, crossing or wandering of one or both eyes, or light sensitivity. In some severe cases, the sign of vision problems may be a regression in overall function or loss of developmental milestones. Ptosis will be seen as a lid droop, and a blocked tear duct will result in daily tearing and discharge.
Any Thoughts for Parents of a Child With Down Syndrome Who Are Concerned About the Eye or Vision?
Dr. Ledoux: Getting regular eye exams is very important in children with Down syndrome because eye disorders are so common and are difficult for the paediatrician to diagnose. Because the examination can be difficult for both the child and the doctor, it is best to have the examination done by an ophthalmologist skilled in dealing with children with developmental delays. Don’t be surprised to find out your child needs glasses; if needed, the glasses will help the vision, and possibly the eye alignment, as well as to help in the development of normal vision pathways in the brain. This will help with your child’s learning and functioning.